Nemours Children’s Hospital (NCH) was awarded The Innovation of the Year in Patient Care award by the Florida Hospital Association (FHA) on Oct. 4 at The Celebration of Service Awards Ceremony in Orlando. NCH was given the award due to their 3D modeling program that has proven to be a significant aid in cancer and cardiac surgeries as well as preoperative interventional radiology.
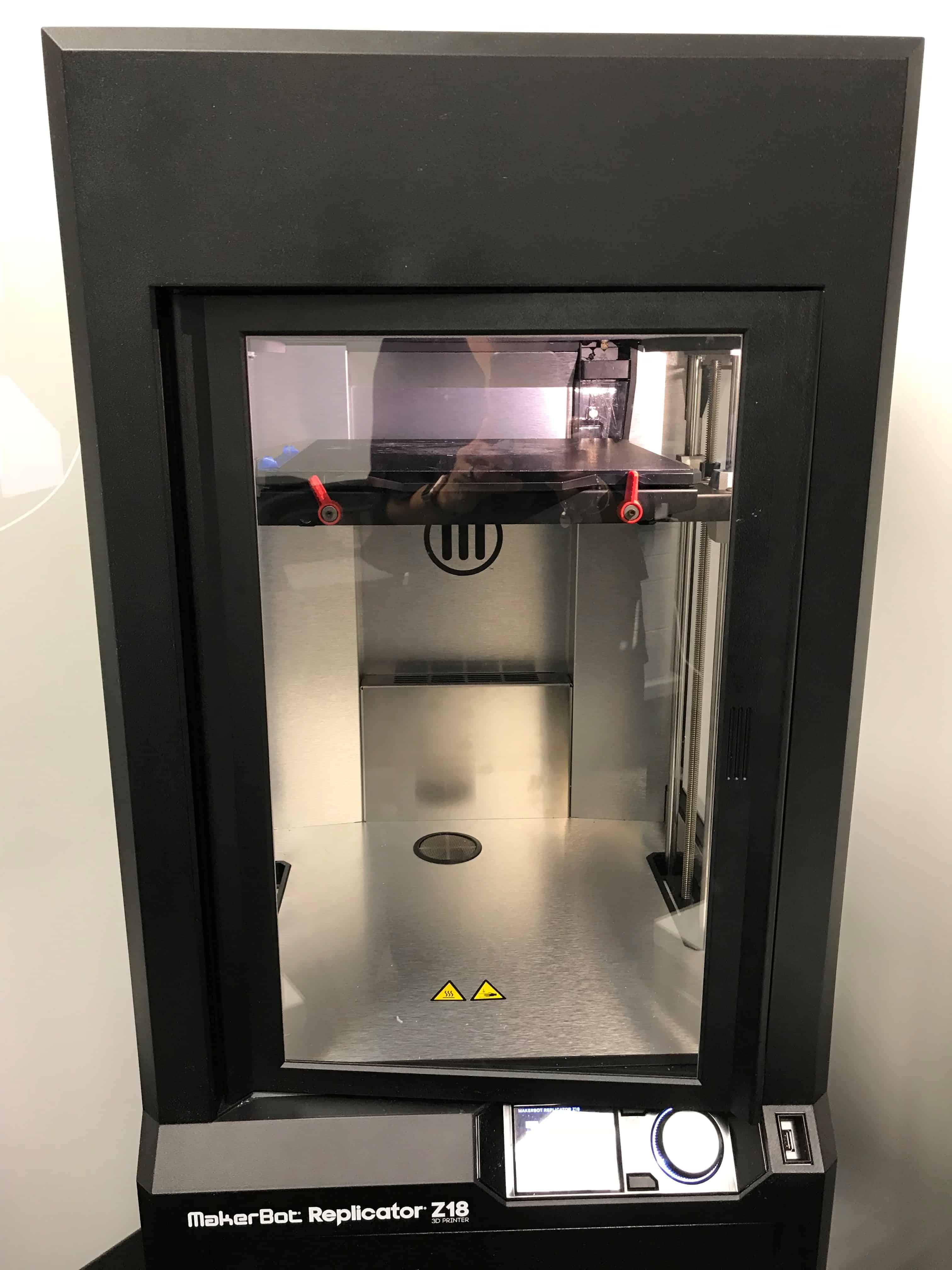
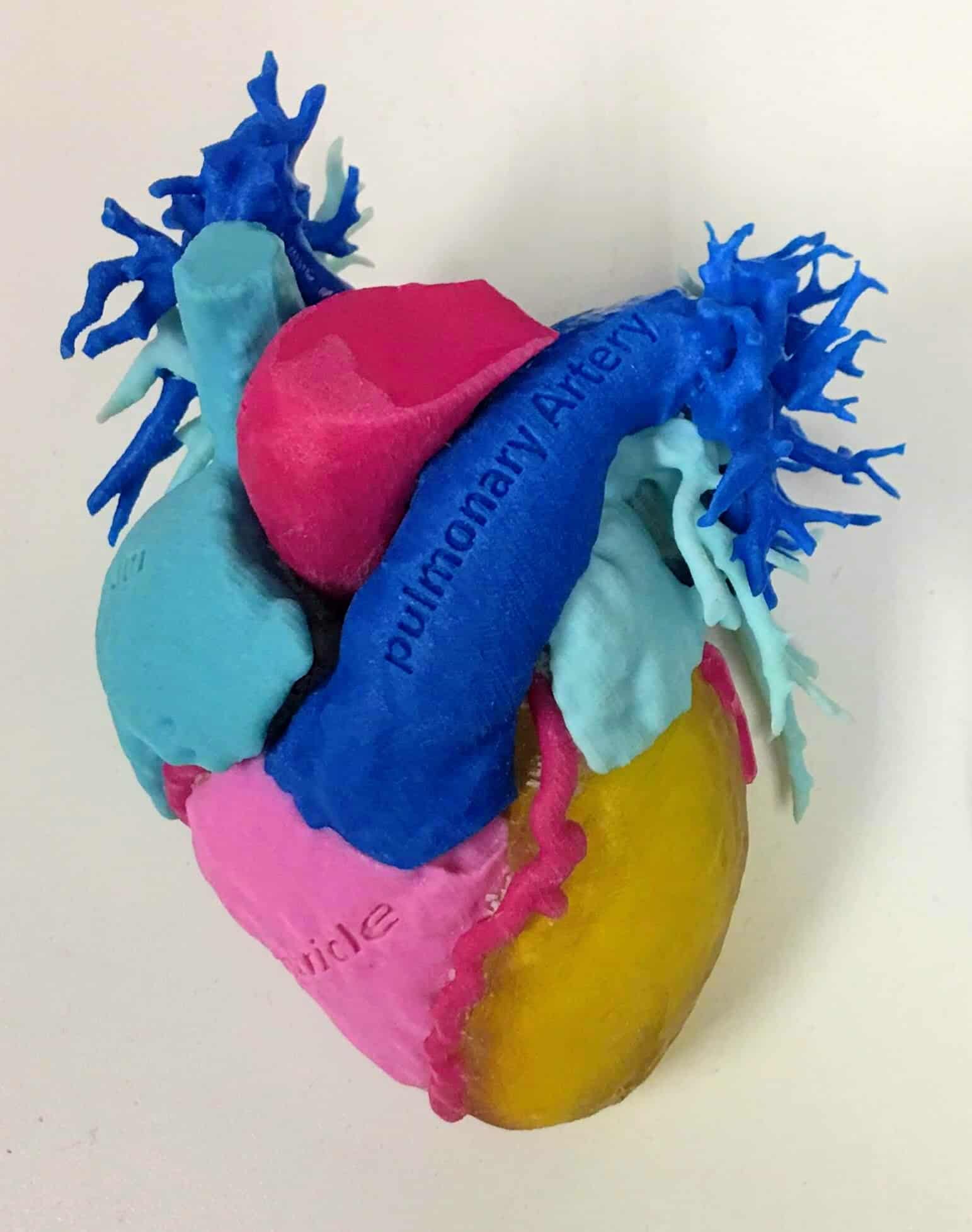
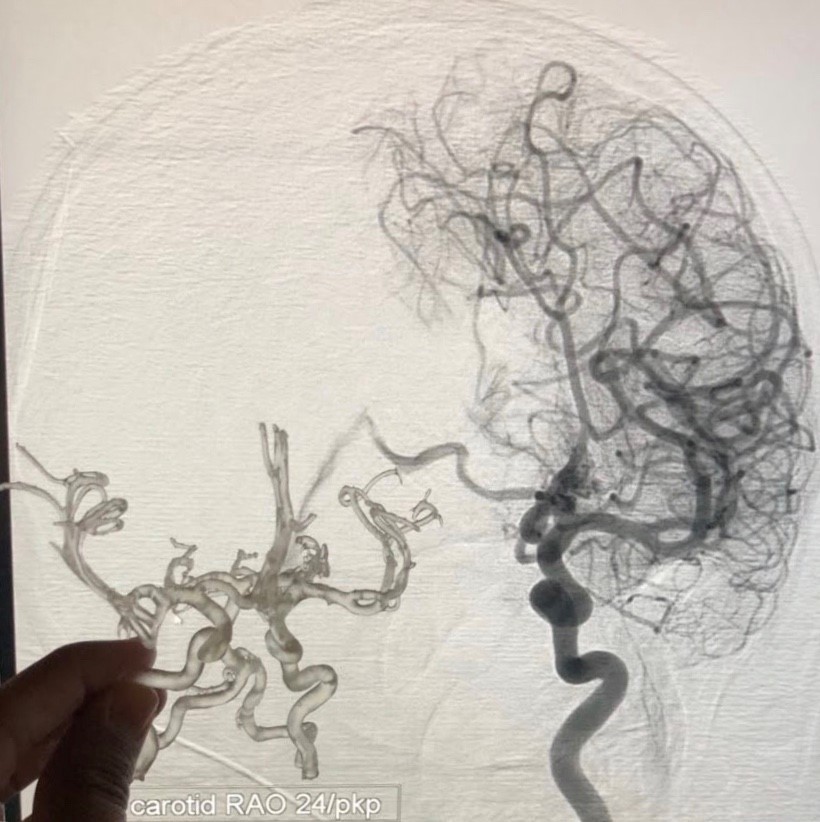
According to the NCH press release, “Utilizing cutting-edge 3D modeling technology, Nemours surgeons, radiologists and proceduralists are using the only FDA-approved segmentation software to plan complex multidisciplinary cases in interventional radiology, cancer surgery, and cardiac surgery.” The 3D models provide reduced procedural times and nearly eliminate unexpected finds in the operating room. This technology offers the opportunity to run simulated surgeries in order to more accurately determine which surgical tools will be needed prior to the actual surgery. As if that weren’t impressive enough, Nemours undertakes these extra steps on behalf of the families as the technology service is not yet covered by insurance plans.
Nonahood News had the opportunity to interview Craig Johnson, the enterprise director of interventional radiology of Nemours Children’s Health System and chair of the department of radiology at Nemours Children’s Hospital.
NHN: How long have you been using the 3D modeling?
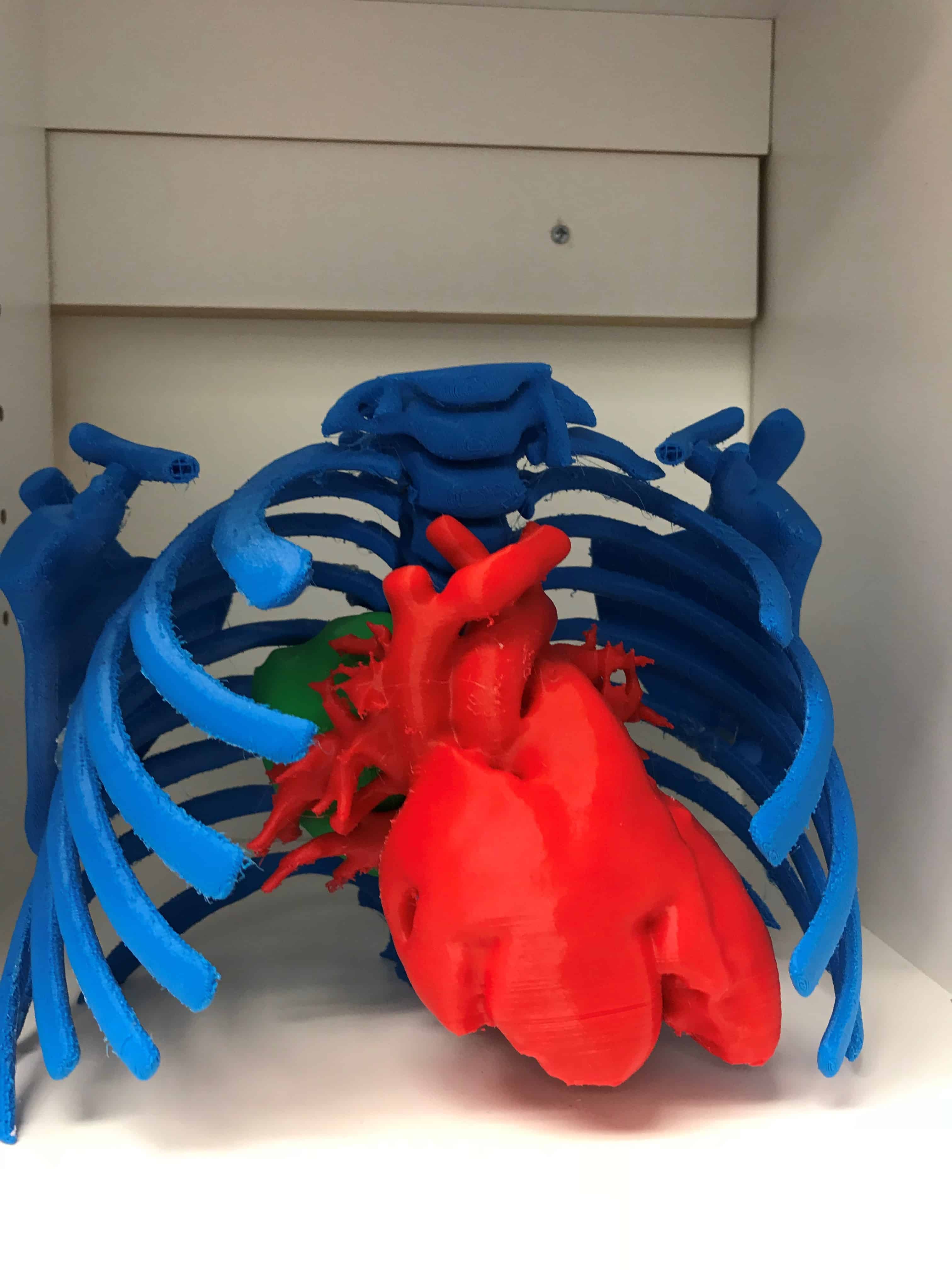
CJ: I think the first one we printed was about three years ago, and those were some of the most basic ones. And then we had a bunch of hurdles that we had to solve on being able to use the technology that we use for MRI scans to convert them into a data set, similar to JPEG converting to a GIF. It’s a very easy process for us to do now, but in the beginning, it wasn’t such an easy process. And then being able to create what we call “segmentation,” which is just 3D representation of all the different organs in the body. Everything from the skin to the rib to the lungs, heart – the entire chest or the entire abdomen and then being able to take pieces of that out that aren’t relevant to the surgical procedure that needs problem-solving from all the subspecialists. And then deciding what to leave in – critical vital structures that we need to decide where we’re going to make the incisions, how we’re going to approach the actual surgeries, and what to look out for complication-wise for the surgeries.
NHN: How many patients has this technology helped so far?
CJ: We’re probably at about 30 now. And we don’t do it for everybody. We certainly do it for complex cases that really need every additional input that we can do. Complex cases such as a new baby born with a complex congenital heart disease; a disorder in which all of the blood vessels in the heart were not formed correctly, inserting into the wrong locations, in which a surgeon would need to cut those vessels and to rearrange inside the chest so the baby can live a normal life for as long as they possibly can. Or the abdominal cancer surgeries where you have a giant tumor that’s growing into adjacent structures and all the things that should be in the abdomen are in abnormal locations, twisted and turned, and its very, very important to know where to cut from, where to not cut to not run into giant blood vessels or uritors that drain the urine and keep the kidneys going. But we’ve printed way more than that – 100, 200 of them. But ones that we’ve actually used to put down in the middle of the table and help the different surgical subspecialist decide on how they’re going to do the procedure in that advanced format, that’s been around 30.
NHN: How accurate are these 3D prints?
CJ: “High fidelity” is the key term. It’s a complete high fidelity system from beginning to end. It is accurate to much less than a millimeter. One period on a piece of paper is one millimeter. It’s accurate to that point. If you came in and we did a whole body scan, we could make a complete replica of your entire cells from top to bottom and it would be the identical height of you, your fingers would be the same size, everything.
NHN: In the future, what would be the next thing Nemours Children’s Hospital is known for in the innovation realm for 3D printing?
CJ: Continuing to advance digital and 3D guidance systems, going into the VR and haptic feedback where you put on gloves that have little sensors and you put on your glasses and you’re in a new world. When you actually shake somebody’s hand in that world, you feel your hand being shaken. That’s [going to] allow to simulate surgeries even better. Right now we have wonderful anatomic info to make decisions on where to cut, but to be able to do more and know more before you actually put the patient to sleep, I think that’s going to become more of the future and make the surgery quicker.
The hospital has received awards every year since opening its doors in 2012, this being the sixth award in six years from FHA and their fifth Innovation of the Year award. To learn more about this unique, personalized and life-saving medical technology using 3D modeling, watch the short video here: nonahood.to/nemours-award.



